What's Happening?
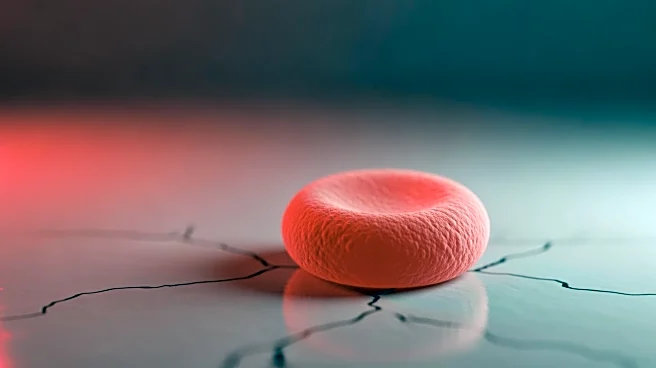
A study led by Isha Jain, PhD, at the Gladstone Institutes, Arc Institute, and University of California, San Francisco, has uncovered a mechanism by which hypoxia, or low oxygen levels, leads to lower blood glucose levels. The research, published in Cell
Metabolism, found that red blood cells (RBCs) in hypoxic conditions metabolize glucose more rapidly, converting it to 2,3-diphosphoglycerate (2,3-DPG), which aids in oxygen release to tissues. This process is facilitated by a metabolic switch involving the protein Band 3. The study suggests that hypoxia reprograms bone marrow to produce glucose-hungry RBCs, contributing to improved glucose tolerance and reduced diabetes risk at higher altitudes.
Why It's Important?
The findings have significant implications for diabetes treatment, as they suggest new therapeutic avenues. By understanding how RBCs contribute to glucose metabolism under hypoxic conditions, researchers can explore potential treatments that mimic these effects. This could lead to innovative therapies for managing blood glucose levels in diabetic patients, potentially reducing reliance on traditional insulin-based treatments. The study also highlights the importance of investigating overlooked physiological mechanisms, which could lead to breakthroughs in understanding and treating metabolic disorders.
What's Next?
Future research may focus on developing therapies that replicate the hypoxic effects on RBCs without requiring actual low-oxygen environments. This could involve engineering RBCs to enhance their glucose uptake or targeting bone marrow to produce more metabolically active cells. Additionally, clinical trials may be necessary to test the safety and efficacy of these potential treatments in humans. The study opens the door to exploring how environmental factors like altitude can influence metabolic health, potentially leading to new public health strategies.