What's Happening?
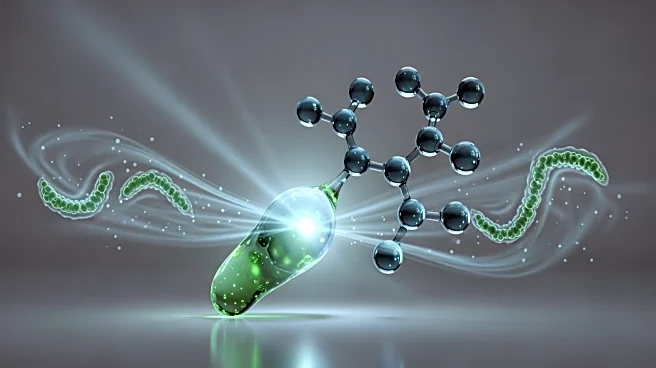
A study published in Nature reveals that a microbiota-dependent bile acid, isolithocholic acid (isoLCA), can reprogram alveolar macrophages to control lung inflammation. The research involved experiments
on mice and human monocyte-derived macrophages, demonstrating that isoLCA can reduce pro-inflammatory responses and neutrophil influx in the lungs. The study suggests that isoLCA influences pathways related to immune response and inflammation, offering a potential therapeutic approach for inflammatory lung diseases. The findings highlight the complex interactions between gut microbiota and lung health, suggesting new avenues for treating conditions like asthma and chronic obstructive pulmonary disease (COPD).
Why It's Important?
This research underscores the significant role of gut microbiota in regulating immune responses beyond the gut, particularly in the lungs. The ability of isoLCA to modulate inflammation could lead to novel treatments for respiratory diseases, which are a major public health concern. Understanding the gut-lung axis opens new possibilities for managing inflammatory conditions through microbiota-targeted therapies. This could revolutionize treatment approaches, reducing reliance on traditional anti-inflammatory drugs and their associated side effects.
What's Next?
Further research is needed to explore the therapeutic potential of isoLCA in human clinical trials. Scientists may investigate the broader implications of microbiota-derived metabolites in other inflammatory diseases. The study could pave the way for developing microbiota-based interventions, potentially leading to personalized medicine approaches in treating lung inflammation.