What's Happening?
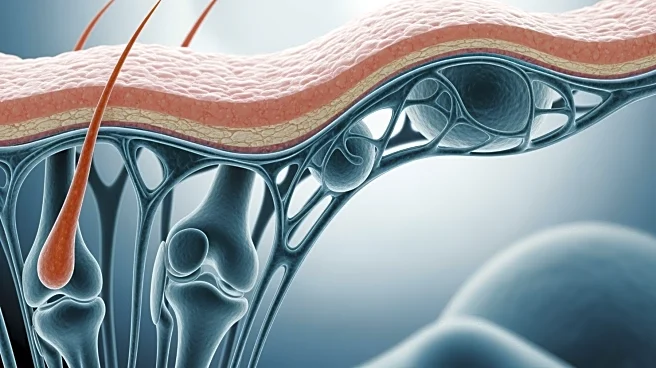
A recent study has uncovered the cellular and molecular mechanisms responsible for the spread of psoriatic disease from the skin to the joints. The research highlights the role of skin-derived myeloid
precursors and joint-resident fibroblasts in this process. The study identifies CD2+MHC-II+CCR2+ myeloid precursors and their interaction with synovial fibroblasts as key factors in the spread of inflammation. The CD200–CD200R1 axis is also highlighted as a pivotal element in this mechanism. The findings suggest that similar to tumor metastasis, the spread of psoriatic inflammation requires migrating cells and a supportive microenvironment. This research opens up new avenues for developing diagnostic and therapeutic strategies aimed at improving patient outcomes.
Why It's Important?
The study's findings are significant as they provide a deeper understanding of the pathogenesis of psoriatic disease, which affects millions of people worldwide. By identifying specific cellular interactions and pathways, the research offers potential targets for new treatments that could prevent or mitigate the spread of inflammation from the skin to the joints. This could lead to improved management of psoriatic arthritis, a condition that can cause severe joint damage and disability. The identification of new therapeutic targets could also lead to the development of more effective drugs, reducing the burden of the disease on patients and healthcare systems.
What's Next?
Future research will likely focus on validating these findings in clinical settings and exploring the development of therapies that target the identified pathways. Clinical trials may be designed to test the efficacy of blocking the CD200–CD200R1 interaction or other identified targets in preventing the spread of psoriatic disease. Additionally, further studies could investigate the role of other cellular and molecular players in the disease's progression, potentially uncovering additional therapeutic targets.
Beyond the Headlines
The study not only advances the understanding of psoriatic disease but also contributes to the broader field of inflammatory diseases. The mechanisms identified may have implications for other conditions characterized by similar patterns of inflammation and tissue migration. This research underscores the importance of a detailed understanding of disease mechanisms in developing targeted therapies, which could revolutionize treatment approaches for various inflammatory diseases.