What's Happening?
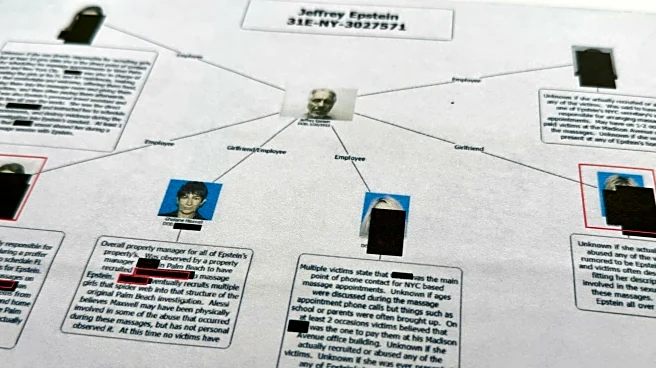
The Centers for Medicare and Medicaid Services (CMS) has announced that Texas is one of six states selected to participate in the WISeR (Wasteful and Inappropriate Service Reduction) Model. This six-year
voluntary program, running from January 1, 2026, to December 31, 2031, aims to modernize Medicare's claims review process using advanced technologies like artificial intelligence and machine learning. The initiative involves private-sector technology firms, such as Cohere Health Inc., which will review specific Medicare services prone to fraud, waste, or abuse. These services include skin and tissue substitutes, electrical nerve stimulator implants, and knee arthroscopy procedures for osteoarthritis. The reviews will be conducted using technology platforms supported by clinical staff, with recommendations for non-payment made by licensed clinicians based on standardized criteria. The model introduces a performance-based incentive structure, where participating firms receive a percentage of savings from reduced unnecessary services.
Why It's Important?
The WISeR Model represents a significant shift in how Medicare manages claims, integrating private-sector innovation directly into federal health oversight. By leveraging technology, the program aims to reduce low-value services, improve patient outcomes, and streamline administrative processes. This initiative could lead to substantial cost savings for Medicare and enhance the efficiency of healthcare delivery. For Texas-based vendors, the model offers new opportunities to engage with Medicare providers, potentially driving demand for digital health tools, clinical decision support, and AI-driven platforms. The program's success could set a precedent for future federal health initiatives, emphasizing the role of technology in healthcare reform.
What's Next?
As the WISeR Model rolls out, participating technology firms will begin implementing their review processes. Healthcare providers in Texas serving Original Medicare beneficiaries will have the option to submit prior authorization requests through model participants. Those who opt out may face post-service reviews to ensure compliance with Medicare rules. The program's performance-based incentives will likely encourage technology firms to optimize their processes, potentially leading to further innovations in claims management. Stakeholders will be closely monitoring the program's impact on service delivery and cost savings, which could influence future policy decisions regarding Medicare and healthcare technology integration.