What's Happening?
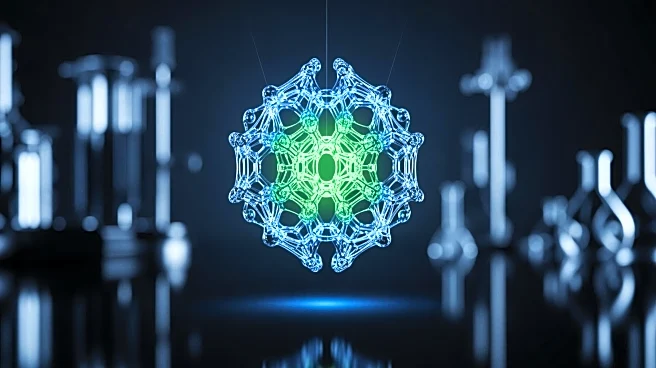
A recent study conducted by IDIBELL, the University of Barcelona, Bellvitge University Hospital, and CIBERDEM has explored the diminishing effectiveness of sulfonylureas, a common class of drugs used to treat type 2 diabetes. Published in the journal Diabetes, Obesity and Metabolism, the research highlights that these drugs can lead to a loss of identity in insulin-producing beta cells, reducing their ability to secrete insulin and potentially accelerating the progression of type 2 diabetes. Sulfonylureas, which have been used since the 1950s, initially help lower blood glucose levels but eventually lose their efficacy, a phenomenon known as secondary sulfonylurea failure. The study found that prolonged exposure to these drugs causes beta cells to lose their functional identity, leading to decreased insulin production and increased cell death.
Why It's Important?
The findings of this study are significant as they provide insight into why sulfonylureas become less effective over time, impacting the management of type 2 diabetes. This loss of drug efficacy can lead to worsening of the disease, affecting millions of patients who rely on these medications for blood glucose control. Understanding the mechanism behind the loss of beta cell identity opens new avenues for research into potential therapies that could reverse this process, offering hope for more effective long-term treatment options. The study underscores the need for continued research into diabetes treatments that can maintain or restore beta cell function, which is crucial for managing the disease and improving patient outcomes.
What's Next?
The study suggests that the loss of beta cell identity is potentially reversible, which could lead to the development of new therapies aimed at restoring the functional identity of these cells. Future research will likely focus on understanding the exact mechanisms of this process and how it can be reversed, potentially leading to innovative treatments that could improve the efficacy of diabetes management. Additionally, the findings may prompt healthcare providers to reconsider the long-term use of sulfonylureas and explore alternative treatment options that do not compromise beta cell function.
Beyond the Headlines
The study raises ethical considerations regarding the continued use of sulfonylureas despite their known limitations and potential harm to beta cell function. It also highlights the importance of personalized medicine in diabetes treatment, where therapies are tailored to individual patient needs and responses. The potential reversibility of beta cell identity loss could shift the focus of diabetes research towards regenerative medicine, offering new hope for patients with type 2 diabetes.