What's Happening?
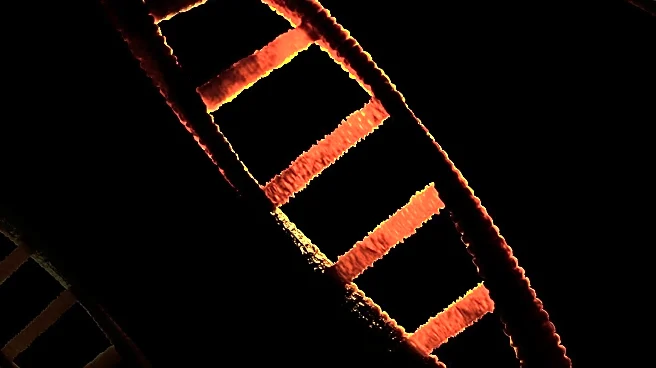
Recent research has identified Z-DNA-binding protein 1 (ZBP1) as a significant factor in exacerbating myocardial ischemia-reperfusion (I/R) injury by inducing noncanonical cardiomyocyte PANoptosis. The study involved time-series RNA-seq analyses on myocardial samples from mice subjected to ischemia followed by reperfusion, revealing a marked increase in ZBP1 expression during the reperfusion phase. ZBP1 was found to drive programmed cell death pathways, including pyroptosis, apoptosis, and necroptosis, in cardiomyocytes. Conditional knockout of ZBP1 in mouse models showed a reduction in these cell death markers and improved cardiac remodeling outcomes. Conversely, overexpression of ZBP1 led to increased cardiac remodeling and heart failure, highlighting its role in cardiomyocyte death.
Why It's Important?
The findings underscore the potential of ZBP1 as a therapeutic target for myocardial I/R injury, a condition that significantly impacts cardiovascular health. By elucidating the mechanisms through which ZBP1 induces cell death, the study opens avenues for developing targeted treatments that could mitigate heart damage and improve recovery outcomes. The research also highlights the broader implications for understanding cell death pathways in cardiac diseases, potentially influencing future drug development and clinical practices aimed at reducing heart failure and improving patient prognosis.
What's Next?
Further research is needed to explore the therapeutic potential of ZBP1 inhibitors in clinical settings. The study suggests that targeting ZBP1 could protect against myocardial injury, and ongoing investigations may focus on developing small-molecule inhibitors to disrupt ZBP1-mediated interactions. Additionally, clinical trials could be initiated to assess the efficacy and safety of such treatments in human patients, potentially leading to new interventions for heart disease management.
Beyond the Headlines
The study raises ethical considerations regarding genetic manipulation and the development of targeted therapies. As research progresses, it will be crucial to address the long-term effects and potential risks associated with inhibiting ZBP1, ensuring that treatments are both effective and safe for widespread use. Moreover, the findings contribute to a deeper understanding of the molecular mechanisms underlying heart disease, which could influence public health strategies and educational efforts aimed at preventing cardiovascular conditions.