The Magnesium Drain
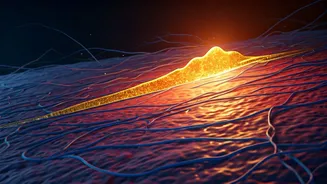
Following the half-century mark, a significant physiological shift occurs, compelling the body to reallocate its magnesium reserves. A neuroscientist highlights
that instead of solely focusing on bone maintenance, the body begins to draw magnesium away from the skeletal system. This isn't a malicious act but rather a survival mechanism, prioritizing vital functions that rely heavily on this mineral, such as nerve transmission and muscle function. As we get older, these cellular processes become even more critical, and the body will ensure they receive adequate magnesium, even at the expense of bone density. This redistribution can have profound implications for bone health, potentially increasing the risk of conditions like osteoporosis if not addressed through dietary or supplemental means.
Vital Functions at Stake
Magnesium is an unsung hero, deeply involved in over 300 enzymatic reactions throughout the body. Its role extends far beyond mere bone structure. It's a key player in maintaining healthy nerve signaling, ensuring that messages travel efficiently between the brain and the rest of the body. Furthermore, magnesium is indispensable for proper muscle contraction and relaxation; without it, muscles could cramp or fail to function correctly. It also plays a part in regulating blood pressure, blood sugar levels, and energy production. When the body reaches a certain age, these fundamental cellular operations are prioritized, leading to the noticeable shift where magnesium is preferentially channeled towards these critical biological processes, even if it means withdrawing it from the bones.
Implications for Bone Health
The consequence of the body's magnesium reallocation after 50 is a direct impact on bone mineral density. Bones are not static structures; they are dynamic, constantly undergoing remodeling. Magnesium is a vital component of the bone matrix, contributing to its strength and resilience. When the body begins to pull magnesium from the bones to support other essential functions, the bone's structural integrity can be compromised. This gradual depletion can lead to weaker bones, making them more susceptible to fractures and increasing the risk of developing osteopenia and, eventually, osteoporosis. This underscores the importance of proactive bone health management as individuals enter their later years, paying close attention to mineral intake.