The Back Pain Conundrum
Chronic low back pain is a pervasive global health issue, affecting individuals across all age groups and placing immense pressure on healthcare systems.
For a significant number of sufferers, this pain becomes persistent, severely impacting their ability to sleep, move freely, and overall quality of life. A significant challenge in managing this condition is the frequent absence of a clear, identifiable structural cause, which complicates the development of effective long-term treatment strategies. This lack of a precise diagnosis often leaves physicians without a definitive target for intervention, leading to a cycle of trial-and-error for patients seeking relief. The economic and personal toll of unmanaged back pain is substantial, underscoring the urgent need for innovative approaches that address the underlying biological mechanisms driving the discomfort. Understanding the intricate interplay between bone health and nerve signaling is crucial for developing targeted therapies.
Hormone's Role in Relief
Groundbreaking research, published in the journal Bone Research, proposes a promising new avenue for combating chronic back pain. The study highlights the potential of hormone-based therapies to alleviate discomfort by inhibiting the aberrant growth of pain-sensing nerves into compromised spinal regions. Spearheaded by Dr. Janet L. Crane at Johns Hopkins University, this work illuminates a previously unrecognized role for bone cells in modulating pain perception during spinal deterioration. Dr. Crane explains that during degeneration, pain nerves infiltrate areas they shouldn't normally occupy, and parathyroid hormone (PTH) has been shown to reverse this process. It achieves this by activating natural cellular signals that effectively guide these nerves away from sensitive zones, thereby reducing pain signals.
PTH and Bone Health
Parathyroid hormone (PTH) is a naturally occurring hormone vital for regulating calcium levels in the body and maintaining bone integrity. Synthetic forms of PTH are already a cornerstone in treating osteoporosis, a condition characterized by weakened bones. Prior research had suggested that these bone-strengthening treatments might also offer pain relief associated with bone damage, but the precise biological mechanisms remained elusive. To unravel this mystery, the research team utilized three distinct mouse models designed to mimic common causes of spinal degeneration: the natural aging process, experimentally induced spinal instability, and an inherited predisposition to bone issues. These models allowed scientists to meticulously observe how degenerative changes in bone structure coincided with alterations in nerve growth patterns within the spine.
Therapeutic Impact Observed
The study involved administering daily injections of PTH to the mice for periods ranging from two weeks to two months, with a control group receiving placebos. Comprehensive analysis using high-resolution imaging techniques revealed significant improvements in the vertebral endplates of PTH-treated mice after one to two months. These crucial structures, situated between the spinal discs and vertebrae, became denser and exhibited enhanced structural stability. These physical enhancements correlated with tangible functional benefits. The treated animals demonstrated a greater tolerance to pressure, a delayed reaction to heat stimuli, and exhibited increased activity levels compared to their untreated counterparts. These findings strongly indicate that PTH treatment not only fortifies bone structure but also directly influences pain perception and mobility.
Curbing Nerve Proliferation
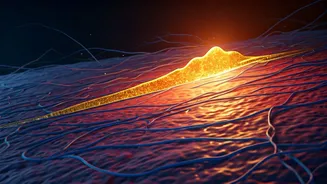
A key focus of the research was the examination of nerve fibers within the spinal tissue. In degenerative spinal conditions, pain-sensing nerves often grow into areas where they are not typically found, a phenomenon known as aberrant innervation, which intensifies sensitivity and exacerbates discomfort. The study clearly demonstrated that PTH treatment significantly curtailed this abnormal nerve growth, as evidenced by reduced levels of specific nerve fiber markers like PGP9.5 and CGRP. This reduction in invasive nerve fibers is a critical factor in mitigating chronic pain. The research further delved into the cellular pathways responsible for this effect, identifying osteoblasts—bone-building cells—as crucial mediators.
The Slit3 Signaling Pathway
Further investigation illuminated the biological mechanism at play: PTH stimulates osteoblasts to release a protein called Slit3. This protein acts as a potent directional cue, effectively signaling pain-sensing nerve fibers to retract from or avoid growing into vulnerable spinal regions. Laboratory experiments corroborated this finding; when nerve cells were cultured with Slit3, their tendency to extend and grow was demonstrably limited, resulting in shorter and less invasive extensions. Conversely, when the Slit3 gene was experimentally removed from osteoblasts in mice, PTH treatment lost its ability to reduce nerve growth or alleviate pain-related behaviors. The researchers also identified another regulatory protein, FoxA2, which appears to play a role in initiating Slit3 production in response to PTH, thus connecting hormonal signals to nerve activity modulation.
Clinical Implications Ahead
Although this significant research was conducted using animal models, the findings hold substantial promise for human health. They may shed light on why individuals undergoing osteoporosis treatment with PTH-based medications often report a reduction in their back pain. The study's authors emphasize that direct clinical trials in humans are essential before these findings can be confidently translated into standard medical practice. Dr. Crane concludes that their research lays the groundwork for future clinical investigations into the effectiveness of PTH as a therapeutic agent for spinal degeneration, potentially offering both disease modification and significant pain relief for patients suffering from chronic low back pain.